If Back Pain Awakens You from Sleep-You May Need to See a Rheumatologist
by Dr. David Borenstein M.D. Medically Reviewed by Dr. C.H. Weaver M.D. Updated 4/2022
Low back pain is the second most common affliction of humankind; only the common cold affects more people. Back pain doesn’t discriminate, people of all ages and genders, and from all walks of life are afflicted with this debilitating discomfort. If you lift, bend, reach, squat, twist, or turn—or even sneeze—you are at some risk for developing back pain.
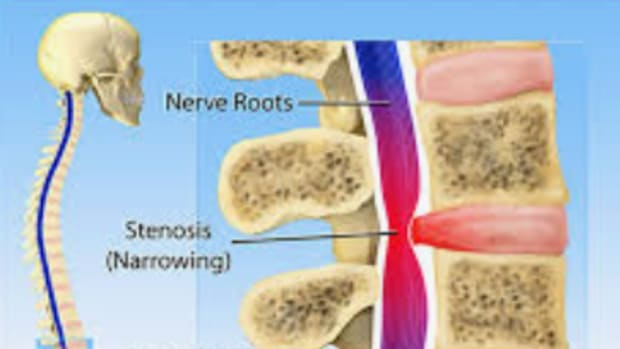
Most low back pain results from mechanical disorders of the spine related to overuse, such as habitually poor posture, or injury or deformity of a portion of the spine, such as a herniated disc. The other 10 to 15 percent of individuals have “medical back pain” caused by systemic illnesses such as nerve damage from diabetes or fibromyalgia or inflammation. These individuals require a more complete evaluation by a rheumatologist.
Back pain sufferers and physicians alike must sort through the events surrounding the development of back pain and each individuals’ unique symptoms in order to determine the cause of the pain and access the best medical professional to help diagnose and treat the problem.
Specific causes of low back pain have reproducible characteristics. For instance, ruptured discs pressing on nerves cause pain that runs from the back to the lower leg and foot.
A study presented at the American College of Rheumatology Annual Meeting has revealed that the most common symptoms in individuals with back pain from inflammatory arthritis are the duration of morning stiffness and pain that wakes an individual from sleep.
Spondylitis is the medical term for inflammatory back pain and it is associated with a number of different characteristics including onset before age 45, prolonged morning stiffness, pain increased at night, increased pain with inactivity and improvement with movement.
RECOMMENDED ARTICLES
HLA-B27 and normal survival
HLA-B27 is a genetic marker that is seen in normal individuals without arthritis and with individuals who are diagnosed with an illness that causes inflammation of the spine, ankylosing spondylitis (AS).
The Importance of the ICD-10 Code for Non-Radiographic Axial Spondyloarthritis
Most patients have minimal interest in the International Classification of Disease (!CD-10) coding manual.
The investigators from Canada asked 234 patients with spondyloarthritis what were their most common symptoms associated with their back pain? The most common symptoms reported were duration of stiffness and nocturnal awakening. Symptoms reported but less often were improvement with exercise, exacerbation with rest, and response to non-steroidal medications.
Ultimately patients with nocturnal awakening and prolonged morning stiffness were more likely to be diagnosed with ankylosing spondylitis, and individuals with these symptoms should self-direct themselves to be evaluated by a rheumatologist instead of a primary care physician or “spine surgeon”.
Reference:
- MaksymowychWP et al: Construct validationof the screening for inflammatory pain in the lower back questionanaire: Data from the screening in axial spondyloarthritis in psoriasis, iritis, and colitis cohort (abstract 658) Arthritis Rheumatol 2018; 70 (suppl 10)